The First Pain
Sarah Jenkins was an active, health-conscious mom with a busy career and family in Austin. One spring morning, a dull stomach cramp woke her up. At first, she brushed it off, blaming stress and a skipped meal.

The pain was mild, coming and going. It seemed like just another minor nuisance that didn’t warrant much attention—at least, not yet.
A Niggling Ache
Over the following months, the ache returned in different forms—sometimes sharp, sometimes dull, usually after lifting or bending. Sarah adapted, working around the discomfort, masking it behind a smile at PTA meetings.


When friends offered advice like changing her diet or taking probiotics, she shrugged it off, convinced it wasn’t anything serious. But deep down, she wondered if something more was going on.
Tests and Dismissals
At her yearly check-up, Sarah brought up her ongoing pain. Her doctor ordered a few routine tests—blood work and an ultrasound. When the results came back normal, he suggested it was likely muscular and recommended physiotherapy.


Sarah left feeling a mix of relief and frustration. The pain lingered, unanswered, and she began to wonder if there was more to it than a simple muscle issue.
An Unsettling Change
The discomfort worsened. Sarah began noticing strange changes—her stomach felt bloated, and clothes that once fit well became tight. She chalked it up to stress or maybe even some extra weight after the holidays.


But she couldn't ignore the constant ache anymore. Sometimes, when she placed her hand over her abdomen, she couldn't shake the feeling that something was wrong.
Family Worry
Mark, Sarah’s husband, noticed the change. She was quieter, more withdrawn, and seemed to have less energy. The kids noticed, too, and asked why she winced when lifting them.

Sarah tried to reassure everyone, but privately, she was growing more anxious. Late at night, she lay awake, clutching a heating pad, unsure of what was really going on inside her body.
The Emergency Visit
One day, the pain became unbearable. It bent Sarah over while she was doing dishes, and Mark rushed her to the ER. After a series of tests and imaging, doctors told her nothing life-threatening was visible.


The diagnosis was vague—“nothing serious,” they said. But Sarah couldn’t shake the feeling that something was being overlooked. They recommended following up with her OB-GYN, leaving her more unsettled than before.
Specialists and Second Opinions
Sarah’s search for answers grew more intense. She saw gastroenterologists, gynecologists, and underwent another round of scans. One radiologist noted an unusual shadow near her lower abdomen, but dismissed it as something benign—maybe scar tissue or a cyst.

The answers remained vague, with every doctor offering a version of “wait and see.” The uncertainty was worse than any diagnosis, and Sarah found herself losing sleep, spiraling into endless research.
The Strain at Home
At home, the weight of uncertainty began to take its toll. Mark picked up extra shifts to cover the extra stress, and Sarah tried to keep things normal for the kids. But the guilt was overwhelming.


She missed events, canceled plans with friends, and felt like a stranger in her own life. The pain remained constant, and the life she’d worked so hard to maintain felt like it was slipping away.
A Missed Opportunity
One day, Sarah recalled a scan where the technicians had misread a calcified shadow. They brushed it off as harmless, but she couldn’t shake the nagging feeling that maybe she had missed an opportunity to push for more.


She began to doubt herself—had she done enough to advocate for her own health? That thought lingered, making her question everything, from her parenting to her career choices.
Rumblings of Fear
At a neighborhood coffee, Sarah overheard a casual conversation about someone’s cancer diagnosis. The comment unsettled her. Could it be? She tried to push the thought aside, but it kept creeping back.


The pain grew worse, and despite reassurances from doctors, Sarah couldn’t ignore the growing suspicion that something was terribly wrong. Fear and uncertainty began to take root, and she realized she couldn’t keep ignoring the shadows inside her.
The DNA Test Decision
After months, a surgeon recommended a diagnostic procedure to sample the mass. The plan included pathology and routine DNA testing on the tissue sample to identify its origin.

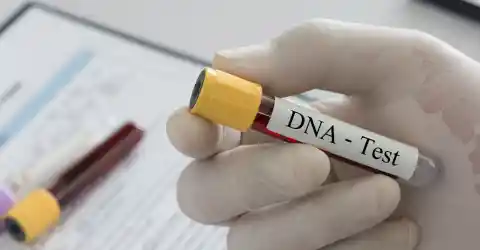
It sounded clinical and ordinary—standard practice to determine whether tissue came from maternal, fetal, or other cells. Sarah agreed reluctantly, nervous about what tests might reveal, but ready to finally know. The day of the procedure felt like holding one breath forever.
Waiting on Results
Recovering at home, Sarah hovered between hope and dread. Lab timelines stretched. Mark tried to be patient for them both, but she could read worry in his pauses.


Friends texted messages of concern; neighbors offered casseroles. Sarah attempted to be present at dinner, but the world felt slightly out of focus. She practiced answers for bad news and good news, rehearsing a life that could bend either way. The unknown tightened like a vise.
Small Signs Return
In the weeks before results, Sarah noticed odd, faint sensations: occasional movements that felt like butterflies low in her belly, a softness that sometimes shifted overnight, odd pelvic cramps like distant thunder.


She shrugged them off—exhaustion, perhaps. Still, she caught herself jotting down dates and times, trying to pattern the sensations. She told no one the whole truth: that a private hope, irrational as it sounded, had begun to flicker in her chest.
Community and Quiet Support
Her church group organized prayer and practical support—groceries, rides, and a standing offer to babysit. Sarah appreciated the kindness but remained guarded about the specifics.


“It’s fine, I’ll be fine” she offered when people asked, and people accepted the simple answer. Mark was her anchor, quietly insisting she rest and follow the doctor’s orders. Yet every kind gesture left her with a cavern of unasked questions. She felt simultaneously loved and exhausted.
The Call That Didn’t Come
A week passed after the biopsy with no phone call. Each ring made her heart leap, then sink when she realized it was nothing important.


The lab said reports can take time. Sarah busied herself—school events, laundry, conference calls—yet the waiting hollowed her out. She began to dread the hospital calls and wonder whether the answer, whatever it was, would make her a different person. The pause itself had become unbearable.
A Late-Night Panic
One night, the cramps returned so fiercely that Sarah could barely breathe. Mark helped her to their car. At the ER, scans were repeated urgently.


Nurses moved with practiced care, and she felt both terrified and oddly calm—this might finally force a definitive answer. A resident reassured her, but the words had no effect on the knot of dread. She thought of the children sleeping at home while a neighbor babysat and braced herself for a life-changing explanation.
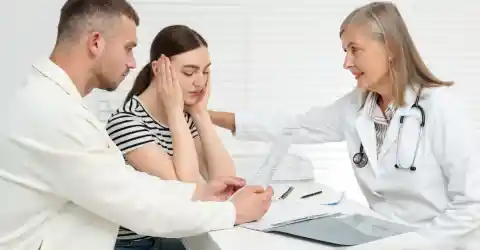
The Specialist’s Tone
The specialist called them in with an expression too careful to be encouraging. He explained they had tissue to analyze, and the pathologist requested DNA testing to determine cellular origin.


“Sometimes tissue can come from many sources,” he said. “We’ll know more soon.” Sarah nodded but barely heard. The clinical calm hid a cliff-edge worry. All the rehearsed responses evaporated. If the sample revealed something unexpected, nothing would ever look the same again.
A Family on Edge
Mark paced the kitchen while Sarah tried to soothe the children and keep her voice steady. “We’ll get through it,” he promised, though his jaw clenched.


The kids sensed the tension and clung a little longer at bedtime. Sarah felt love fold around her like a brittle, precious thing. She had imagined many outcomes—cancer, cyst, scar tissue—but never, even in the wildest hours, what would unfold when the lab report finally arrived.
The Phone Rings
The lab called early in the morning, and Sarah’s hands shook as she took the call. “Your pathologist has requested a consultation. The DNA results need review.” The voice was formal, careful.


Sarah’s vision tunneled. “When can we come in?” she asked, voice small. “We’ll schedule you today,” they said. A rush of cold replaced fear: the appointment would make the unknown known. She hung up and sat in the silence, the house unbearably loud with its ordinary noise.
The Impossible Truth
The pathologist sat across from Sarah and Mark, eyes steady. “Your tissue contains fetal DNA,” she said softly. “We identified genetic markers that don’t match your own. In other words, you have retained fetal tissue.”


The doctor explained a rare medical phenomenon—when a pregnancy implants outside the uterus (an abdominal or ectopic pregnancy), the fetus can die and be too large to be reabsorbed. The body sometimes calcifies the remnant to isolate it—a lithopedion, or ‘stone fetus’—allowing it to remain for years. Recent medical literature documents retained calcified fetal remnants lasting decades, with retention times reported from a few years to many decades.
How It Happens
The doctor continued gently: an abdominal ectopic pregnancy can progress undetected if it doesn’t cause immediate catastrophic bleeding. When the fetus dies and cannot be expelled or reabsorbed, the immune system may deposit calcium around it, essentially “walling it off.”


This calcification prevents infection and inflammation, and a remnant can remain asymptomatic for years. Though extremely rare, fewer than a few hundred cases have been reported worldwide; clinicians rely on imaging and pathology, including DNA testing, for diagnosis.
The Shock and Relief
The room swam for Sarah—shock, horror, then an odd, fragile relief that the mystery had an explanation. She hadn’t been imagining the sensations; there truly had been something living inside her once, now transformed by the body’s defenses.


Mark held her hand tightly, tears wet on his knuckles. “You weren’t alone,” he whispered. The diagnosis was medically staggering but also oddly merciful: she hadn’t been ignoring symptoms—her body had protected her from worse.
Choices and Risks
Doctors discussed options: surgical removal versus careful monitoring. Removal carried risks—surgery in the abdomen with adhesions and scar tissue could cause bleeding or damage—but could relieve symptoms and remove unsettling physical evidence.


Alternatively, leaving the calcified remnant in place might be safer for some patients if it’s stable and not causing problems. Sarah and Mark weighed options with the medical team, fearing risk to her health but longing for closure.
The Aftermath
They chose surgery after a multidisciplinary review. In the operating room, the surgeon described dense calcified tissue adherent to the bowel; careful dissection freed the remnant.


Recovery was slow but steady. Pathology confirmed the clinical diagnosis. Emotionally, Sarah cycled between grief—for the tiny life she never knew—and gratitude for modern medicine’s ability to finally name her condition. The family processed the impossible truth together, learning to hold space for complexity and sorrow.
A New Chapter
Months later, Sarah stood in her kitchen with Mark, watching their children laugh at homework. The scars—both physical and emotional—faded slowly, but she felt lighter. She spoke openly with friends and the community about the importance of advocating for one’s health.


The experience reshaped priorities: deeper checkups, clearer communication, and an appreciation that bodies sometimes keep secrets. Sarah carried memory and meaning forward, grateful for answers and for the family who held her through the impossible.